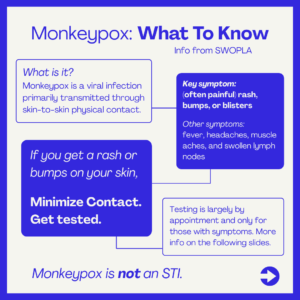
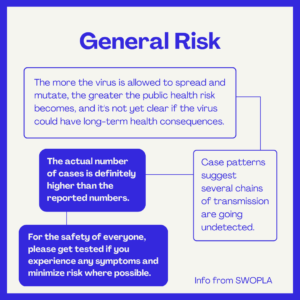
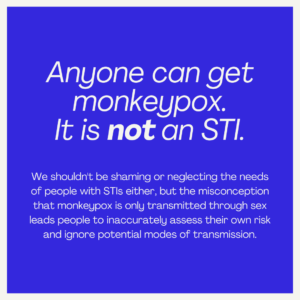
More bad news, sorry. You’ve probably heard by now that there has been an mpox, formerly known as monkeypox, outbreak in the US. The current outbreak was first detected among men who have sex with men, which has led institutions and people to frame mpox as an STI that primarily concerns the LGBTQ+ community. Mpox is not an STI, and anyone can get it.
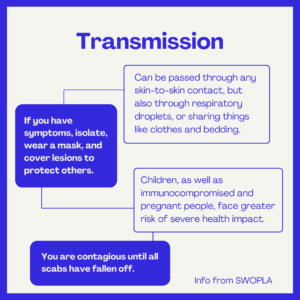
Mpox is transmitted nonsexually. Mpox can be transmitted through the air. Scapegoating marginalized people when fascists are already advancing their attacks on the queer community will lead to violence.
This is the best, most helpful, information we can provide, but personal responsibility is a failing public health model. We need a real government response. The vaccine already exists. Treatment to reduce symptoms and shorten necessary isolation periods exists. This is a solvable problem if we demand the government actually make use of the solutions it has on hand.
But for now, protect yourselves in the ways you can.
Anyone who requests the vaccine can get it without disclosing personal risk info. You should get both doses for the best protection. Make appointments here.
Testing and other info from the LA Public Health Department here.
More images of lesions from the CDC here.
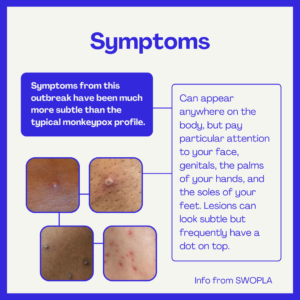
Mpox lesions don’t have a consistent look. They can appear like pimples, blisters, or ingrown hairs, but you know what kinds of pimples and ingrowns you tend to get and where so you’re going to be the best judge of if a spot is unusual for you.
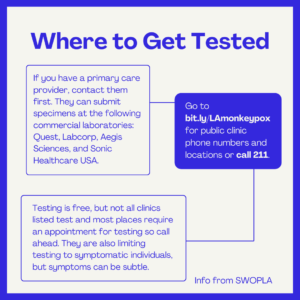
Last we called, Central Health Center and Ruth Temple Health Center were the two on the DPH Sexual Health Clinic list that were not testing for mpox. If you find out this or any other info has changed, let us know.
Some clinics are also not testing people who have insurance. They will tell you that insured people have to go to an Urgent Care center, but many Urgent Care centers are not testing for mpox. You can call around to find one that is or you can go to the ER, but expect to wait.
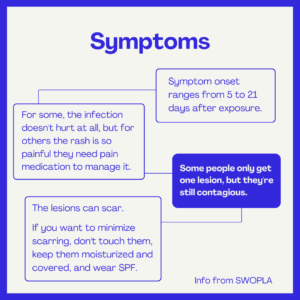
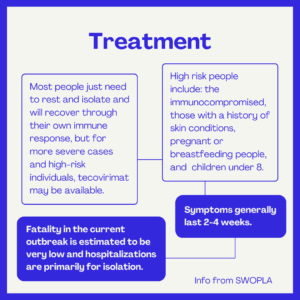
If you test positive, the recommended isolation period is 21 days.
Symptom management guidelines from the Nigeria Center for Disease Control:


More on tecovirimat. If you have a severe case or are high risk, talk to your primary care doctor. All providers can prescribe tecovirimat, they just have to fill out the required EA-IND forms, but these can be submitted to the CDC after treatment has started. Tecovirimat treatment can begin as soon as the doctor obtains signed informed consent from the patient.
If you don’t have a primary care doctor, the Department of Public Health is following all positive cases and will reach out and get you treatment if you need it.
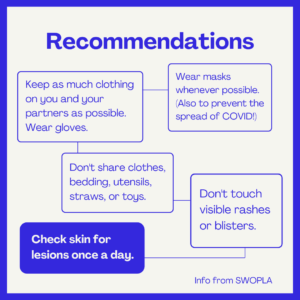
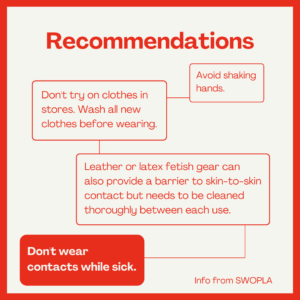
Clothing can also become contaminated with the virus. Change clothes between clients if possible, avoid touching the outside of your garments.
And a short thread on messaging and risk.
*Post has been edited to reflect the World Health Organization’s transition to “mpox” instead of “monkeypox”.
